Virology
Herpesviridae
About herpesviridae
After primary infection and the patient is supposedly cured from the symptoms, the virus remains latent in the body until some factors such as age, stress, long exposure to sunlight and menstrual periods causes its reactivation.
During the term in which it is latent, there are no symptoms displayed. When the latent virus reactivates, it is known as secondary infection. Reactivation however, may result in the development of other diseases.
Herpes means ‘to creep upon’ in Greek. It is given that, because the virus ‘hides’ itself in the nerve tissues during the latent period before reactivation. Herpes also causes viral encephalitis (acute inflammation of the brain) or brain damage if passed from mother to child at childbirth.
There is currently no cure or vaccination for herpes and is labeled as one of the toughest virus to control as infection with herpes, especially HSV-1, is universal.
During the term in which it is latent, there are no symptoms displayed. When the latent virus reactivates, it is known as secondary infection. Reactivation however, may result in the development of other diseases.
Herpes means ‘to creep upon’ in Greek. It is given that, because the virus ‘hides’ itself in the nerve tissues during the latent period before reactivation. Herpes also causes viral encephalitis (acute inflammation of the brain) or brain damage if passed from mother to child at childbirth.
There is currently no cure or vaccination for herpes and is labeled as one of the toughest virus to control as infection with herpes, especially HSV-1, is universal.
Structure of the Herpes virus genome
The morphology of all herpes viruses is more or less similar and sometimes even identical. The herpes virus has a linear double-stranded (ds) DNA and is thus from class 1 of the Baltimore’s classification. It is a concentric virion meaning that, the layers of structure in the virus share the same centre and axis with each other.
The structure of the virus consist of a protein based icosahedral capsid that encloses its linear ds DNA. This capsid is surrounded by a layer of amorphous proteins called the tegument. The protein atoms here are not arranged in orderly repeating pattern as in crystalline solids where long-range order is required. Then, both are enclosed by a lipid bilayer membrane termed the envelope, where the outer layer is dotted with glycoprotein like villi.
It has three origins of replication (ORI) meaning that, there are three areas in the DNA where the DNA is recognized by replication initiator proteins and separated into two strands to start a replication fork where DNA synthesis happens.
It has three origins of replication (ORI) meaning that, there are three areas in the DNA where the DNA is recognized by replication initiator proteins and separated into two strands to start a replication fork where DNA synthesis happens.
Replication
The DNA of the herpes virus only transcribes and replicates in the nucleus of the host cell and is thus nuclear-replicating. Infection begins when the virus comes in contact with a cell at specific receptor on the cell surface membrane. There, the glycoprotein on the virus’s lipid bilayer envelope will bind with the receptors of the to-be-host cell and the virus DNA would enter the nucleus of the host cell.
Pathogenesis
There are 7 distinct viruses in the herpes virus family that causes diseases. 3 of them are:
1. Herpes simplex viruses
(a) HSV1
(b) HSV2
2. Varicella Zoster virus
(a) Varicella
(b) Herpes Zoster
3. Epstein-Barr Virus (EBV)
1. Herpes simplex viruses
(a) HSV1
(b) HSV2
2. Varicella Zoster virus
(a) Varicella
(b) Herpes Zoster
3. Epstein-Barr Virus (EBV)
1. Herpes simplex virus
· It consist of herpes simplex virus 1 (HSV-1) and herpes simplex 2 (HSV-2).
· Symptoms produced for both are asymptomatic and similar to each other although severity may differ. HSV-1 is the main cause for orofacial infections whereas HSV-2 is genital herpes.
· It consist of herpes simplex virus 1 (HSV-1) and herpes simplex 2 (HSV-2).
· Symptoms produced for both are asymptomatic and similar to each other although severity may differ. HSV-1 is the main cause for orofacial infections whereas HSV-2 is genital herpes.
HSV-1
Primary and recurrent infection occurs for HSV-1. Primary infection can range from orofacial lesions like cold sores and blisters around the mouth/gum, eyes and face that last for about 2-3 weeks to swollen lymph nodes, fever, muscle aches and headaches.
Recurrent infections are more common in HSV-1 than HSV-2.
Recurrent infections are more common in HSV-1 than HSV-2.
HSV-2
Primary infection last for 2-3 weeks. There is formation of inflamed pastules and vesicles that appear a week after sexual infection. Burning and itching sensations at the genital/anal areas will be experienced as well as pain when urinating. Other common symptoms include foul-smelling discharge from vagina (female) and penis(male), swollen lymph nodes, fever, muscle and headaches.
Unlike HSV-2 which is transmitted sexually, HSV-1 is not sexually transmitted. Rather, it can be transmitted when the virus comes in contact with abraded skin or oral mucosa.
Control for HSV-1/2
Since there is no cure, early treatment may reduce the number of latent of virus in the body and in doing so, reduce the chances for reactivation. Reduce/avoid risky sexual contact.
2. Varicella Zoster Virus
· It is divided into two clinical entities: Varicella and Herpes zoster.
· Varicella is associated to the cause of chicken pox where else Herpes zoster is associated with shingles.
· Chicken pox is the primary infection of the varicella zoster virus while shingles is the secondary infection.
· People that have been vaccinated against chicken pox when they were children have lower chances of developing shingles.
· It is divided into two clinical entities: Varicella and Herpes zoster.
· Varicella is associated to the cause of chicken pox where else Herpes zoster is associated with shingles.
· Chicken pox is the primary infection of the varicella zoster virus while shingles is the secondary infection.
· People that have been vaccinated against chicken pox when they were children have lower chances of developing shingles.
As stated above, the virus ‘hides’ in the nervous system of the patient after the symptoms have been cured, reactivating only in the later stages of life. Its genome morphology is similar to that of the herpes simplex and is susceptible to disinfectants. Although there is vaccination for the Varicella Zoster virus, the effectiveness of the immunity it provides might dwindle overtime and a second dose maybe required to maintain the immunity levels in the body.
The virus is dangerous in pregnant women because it can be passed to the child or even affect the nervous system of the child, causing development of the Guillain Barre syndrome where the child would suffer extreme pain on the slightest touch.
The virus is dangerous in pregnant women because it can be passed to the child or even affect the nervous system of the child, causing development of the Guillain Barre syndrome where the child would suffer extreme pain on the slightest touch.
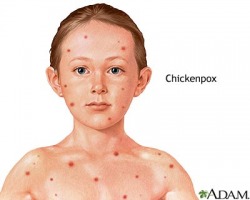
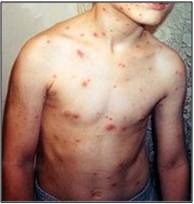
(a) Clinical features of Varicella
Chicken pox only develops around 2-3 weeks after infection is highly contagious during the first few days after rash appears. Primary infection of chicken pox will give lifelong immunity against chicken pox but does not prevent shingles from developing. Adults are more likely to suffer from more severe effects of chicken pox than children if they have not been infected during childhood.
Infection is usually indicated by the distinctive itchy rash that eventually forms blisters (lesions) all over the body and become scabs. It is accompanied by fever and general malaise (the feeling of feeling unwell). Scratched lesions may lead to secondary infection. Scarring may develop depending on seriousness.
Chicken pox only develops around 2-3 weeks after infection is highly contagious during the first few days after rash appears. Primary infection of chicken pox will give lifelong immunity against chicken pox but does not prevent shingles from developing. Adults are more likely to suffer from more severe effects of chicken pox than children if they have not been infected during childhood.
Infection is usually indicated by the distinctive itchy rash that eventually forms blisters (lesions) all over the body and become scabs. It is accompanied by fever and general malaise (the feeling of feeling unwell). Scratched lesions may lead to secondary infection. Scarring may develop depending on seriousness.
It can be spread by direct contact with infected people as well as contact with secretions from the lesions on the skin. It can also be spread via the respiratory track from sneezing or coughing.
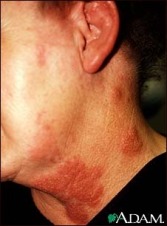
(b) Clinical features of Shingles
Shingles show different symptoms as compared to chickenpox. Painful rash and eventually lesions is experienced. This is caused by infection of nerve axons under the skin since the virus ‘hides’ in nerve cells during its latent period.
Shingles show different symptoms as compared to chickenpox. Painful rash and eventually lesions is experienced. This is caused by infection of nerve axons under the skin since the virus ‘hides’ in nerve cells during its latent period.
Headache, fever, malaise, burning pain, itching, numbness, sudden short outburst of pain and in some serious cases, loss of sight and hearing.
Control for Varicella Zoster virus
· Stay away from infected people.
· Get vaccinated.
· Get vaccinated.
3. Epstein-Barr virus
· Infection is widespread like HVS with almost 100% of the adult population infected due to kissing and close proximity. The EBV test is tested positive almost universally and most children have already been infected by 18 months of age.
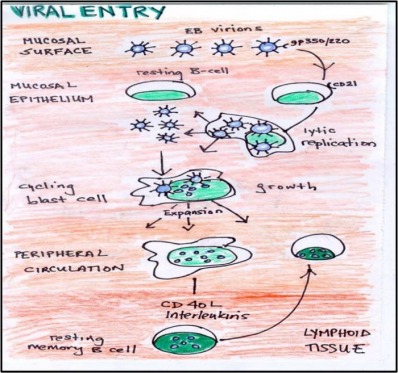
· Instead of remaining latent in the nerve cells like the HVS and VZV, it ’hides’ in the B lymphocytes of the host. The virus is mostly spread via contact with saliva of infected people and is almost impossible to prevent the spreading as the saliva of healthy people also contain the virus. Transmission via blood or respiratory track is uncommon.
· The virus can cause infectious mononucleosis aka glandular fever.
· Infection is widespread like HVS with almost 100% of the adult population infected due to kissing and close proximity. The EBV test is tested positive almost universally and most children have already been infected by 18 months of age.
· Instead of remaining latent in the nerve cells like the HVS and VZV, it ’hides’ in the B lymphocytes of the host. The virus is mostly spread via contact with saliva of infected people and is almost impossible to prevent the spreading as the saliva of healthy people also contain the virus. Transmission via blood or respiratory track is uncommon.
· The virus can cause infectious mononucleosis aka glandular fever.
Clinical features of EBV
It has an incubation period of 4-7 weeks and acute infection does not last for more than 4 months, chronic infection last for more than 6 months. Some symptoms would include fever, sore throat, malaise, tiredness, swollen lymph glands and atypical lymphocytosis (increase in the amount of lymphocytes in the blood) in the peripheral blood.
The virus can also cause infectious mononucleosis aka glandular fever. Symptoms such as fever, fatigue, sore throat, weight loss, malaise. Development of jaundice and hepatitis (inflammation of liver cells) may occur.
The virus can also cause infectious mononucleosis aka glandular fever. Symptoms such as fever, fatigue, sore throat, weight loss, malaise. Development of jaundice and hepatitis (inflammation of liver cells) may occur.
Control
· No vaccines are available.
· Reduce or avoid risky behaviour.
· Reduce or avoid risky behaviour.
Diagnosis
· Virus culture.
· Use antigen tests such as the Enzyme Link Immuno Assay.
· Blood tests such as serology.
· Electron microscopy for direct detection.
· A positive test would show an increase of certain atypical while blood cells in a person infected with EBV. Detection of IgG and IgM against certain antigens for each of the virus.
· Use antigen tests such as the Enzyme Link Immuno Assay.
· Blood tests such as serology.
· Electron microscopy for direct detection.
· A positive test would show an increase of certain atypical while blood cells in a person infected with EBV. Detection of IgG and IgM against certain antigens for each of the virus.