Virology
Latency of Animal Viruses
Some double-stranded DNA animal viruses (such as the herpes viruses and the retroviruses) are able to remain latent within infected host cells for long periods of time without replicating or causing harm. Some of these viruses remain latent within the cytoplasm of the host cell, whereas others are able to integrate their DNA into the chromosomes of the host cell. When the virus DNA is incorporated into the DNA of the host cell, it is called a provirus.
Viral latency is thought to result primarily from the lack of production of specific host cell proteins that are required for the activation of the viral genes responsible for turning on viral replication. As long as these specific host cell proteins are not being made by the host cell, the virus can’t replicate. However, because the virus is inside the infected cell, it also can’t be removed by the body’s immune responses, and the person may carry the virus throughout their life.
Subsequent activation of the host cell’s DNA in response to extracellular stimuli, however, can lead to synthesis of the specific host cell proteins required by the virus and these proteins now activate the viral genes leading to a burst of viral replication via the productive life cycle.
Viral latency is thought to result primarily from the lack of production of specific host cell proteins that are required for the activation of the viral genes responsible for turning on viral replication. As long as these specific host cell proteins are not being made by the host cell, the virus can’t replicate. However, because the virus is inside the infected cell, it also can’t be removed by the body’s immune responses, and the person may carry the virus throughout their life.
Subsequent activation of the host cell’s DNA in response to extracellular stimuli, however, can lead to synthesis of the specific host cell proteins required by the virus and these proteins now activate the viral genes leading to a burst of viral replication via the productive life cycle.
EXAMPLES:
Herpes viruses are often latent in some cell types, but productive in others.
- Herpes simplex type 1 (HSV-1): usually causes fever blisters or oral herpes.
- Herpes simplex type 2 (HSV-2): usually causes genital herpes.
- Epstein-Barr virus (EBV): causes infectious mononucleosis and plays a role in certain cancers.
- Varicella-zoster virus (VZV): causes chickenpox and shingles.
- Cytomegalovirus (CMV): causes a variety of infections in immunosuppressed persons, and also a leading cause of birth defects.
- Herpes simplex type 1 (HSV-1): usually causes fever blisters or oral herpes.
- Herpes simplex type 2 (HSV-2): usually causes genital herpes.
- Epstein-Barr virus (EBV): causes infectious mononucleosis and plays a role in certain cancers.
- Varicella-zoster virus (VZV): causes chickenpox and shingles.
- Cytomegalovirus (CMV): causes a variety of infections in immunosuppressed persons, and also a leading cause of birth defects.
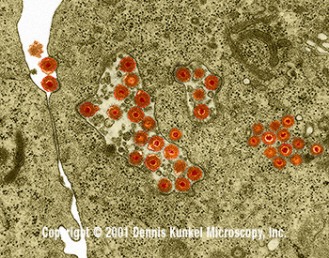
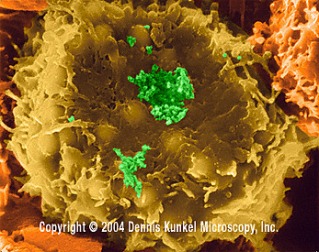
Caption: Herpes simplex virus (HSV-2, DNA virus) in cellular vacuoles and cytoplasm of peripheral blood lymphocyte (Herpesviridae Family). Two virus particles are seen adjacent to the cell membrane in the upper left of the image. The membrane near each virus is depressed and clatharin coated. This represents the classical receptor mediated endocytosis of virus particles. Herpes simplex is a viral infection. HSV-2 causes most of the genital herpes cases.
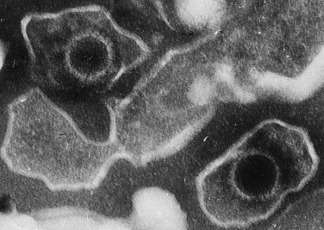
Caption: Electron microscopic image of two Epstein Barr Virus (EBV) virions (viral particles) loosely surrounded by the membrane envelope.
Retroviruses are a group of RNA viruses such as the Human Immunodeficiency Virus (HIV) and Human T-Lymphotropic Viruses (HTL V), that use a unique enzyme called reverse transcriptase to produce a double-stranded DNA intermediate molecule during replication.
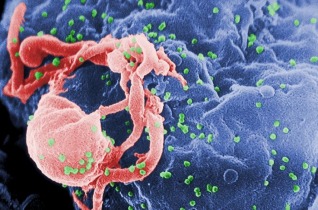
Caption: Scanning electron micrograph of HIV-1 budding (in green) from cultured lymphocyte. Multiple round bumps on cell surface represent sites of assembly and budding of virions.
Caption: Human T lymphocyte with HTLV-1 infection. The virus is centrally located in a large clump (RNA virus, Retroviridae Family).
Relationship between Microbes and Host
‘Normal’ Microflora (Commensal microflora)
In a healthy animal, the internal tissues (blood, brain, muscle, etc.) are normally free of microorganisms. However, the surface tissues (skin and mucous membranes) are constantly in contact with environmental organisms and become readily colonized by various microbial species. The normal flora of humans consists of a few eukaryotic fungi and protists, but bacteria are the most numerous and obvious microbial components of the normal flora.
In a healthy animal, the internal tissues (blood, brain, muscle, etc.) are normally free of microorganisms. However, the surface tissues (skin and mucous membranes) are constantly in contact with environmental organisms and become readily colonized by various microbial species. The normal flora of humans consists of a few eukaryotic fungi and protists, but bacteria are the most numerous and obvious microbial components of the normal flora.
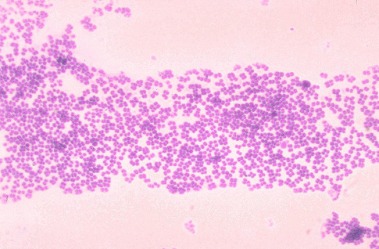
Caption: Gram stain of a species of Micrococcus, commonly isolated from the skin and nasal membranes of humans.
Commensal microflora (normal microflora, indigenous microbiota) consists of those micro-organisms, which are present on body surfaces covered by epithelial cells and are exposed to the external environment (gastrointestinal and respiratory tract, vagina, skin, etc.).
The number of bacteria colonising mucosal and skin surfaces exceeds the number of cells forming human body. Commensal bacteria co-evolved with their hosts, however, under specific conditions they are able to overcome protective host responses and exert pathologic effects. Resident microflora contains a number of components able to activate innate and adaptive immunity. Unlimited immune activation in response to signals from commensal bacteria could pose the risk of inflammation; immune responses to mucosal microbiota therefore require a precise regulatory control. The mucosal immune system has developed specialised regulatory, anti-inflammatory mechanisms for eliminating or tolerating non-dangerous, food and airborne antigens and commensal micro-organisms (oral, mucosal tolerance). However, at the same time the mucosal immune system must provide local defense mechanisms against environmental threats (e.g. invading pathogens).
Regulation of microflora composition (e.g. by probiotics and prebiotics) offers the possibility to influence the development of mucosal and systemic immunity but it can play a role also in prevention and treatment of some diseases.
The number of bacteria colonising mucosal and skin surfaces exceeds the number of cells forming human body. Commensal bacteria co-evolved with their hosts, however, under specific conditions they are able to overcome protective host responses and exert pathologic effects. Resident microflora contains a number of components able to activate innate and adaptive immunity. Unlimited immune activation in response to signals from commensal bacteria could pose the risk of inflammation; immune responses to mucosal microbiota therefore require a precise regulatory control. The mucosal immune system has developed specialised regulatory, anti-inflammatory mechanisms for eliminating or tolerating non-dangerous, food and airborne antigens and commensal micro-organisms (oral, mucosal tolerance). However, at the same time the mucosal immune system must provide local defense mechanisms against environmental threats (e.g. invading pathogens).
Regulation of microflora composition (e.g. by probiotics and prebiotics) offers the possibility to influence the development of mucosal and systemic immunity but it can play a role also in prevention and treatment of some diseases.
Virus Host Relationship
Commensalism
Relationship between two organisms in which one benefits but the other is unaffected.

Caption: Barnacles are highly sedentary crustaceans that must attach themselves permanently to a hard substrate, such as rocks, shells, whales, or anything else they can gain a foothold. When they attach to the shell of a scallop, for instance, barnacles benefit by having a place to stay, leaving the scallop presumably unaffected.
Mutualism
Biological interaction between two organisms, where each individual derives a fitness benefit.
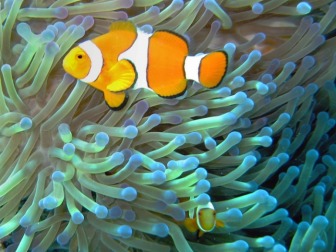
Caption: One example is the relationship between sea anemone and anemonefish (clownfish): the anemones provide the fish with protection from predators (which cannot tolerate the stings of the anemone's tentacles), and the anemonefish defend the anemones against butterflyfish which eat anemones.
Parasitism
Relationship between two organisms in which one benefits, whereas the other is harmed.
Parasites are classified based on their interactions with their hosts and on their life cycles.
Those that live on its surface are called ectoparasites (e.g. some mites) and those that live inside the host are called endoparasites (e.g. hookworms). Endoparasites can exist in one of two forms: intercellular (inhabiting spaces in the host’s body) or intracellular (inhabiting cells in the host’s body). Intracellular parasites, such as bacteria or viruses, tend to rely on a third organism which is generally known as the carrier or vector. The vector does the job of transmitting them to the host. An example of this interaction is the transmission of malaria, caused by a protozoan of the genus Plasmodium, to humans by the bite of an anopheline mosquito.
Parasites are classified based on their interactions with their hosts and on their life cycles.
Those that live on its surface are called ectoparasites (e.g. some mites) and those that live inside the host are called endoparasites (e.g. hookworms). Endoparasites can exist in one of two forms: intercellular (inhabiting spaces in the host’s body) or intracellular (inhabiting cells in the host’s body). Intracellular parasites, such as bacteria or viruses, tend to rely on a third organism which is generally known as the carrier or vector. The vector does the job of transmitting them to the host. An example of this interaction is the transmission of malaria, caused by a protozoan of the genus Plasmodium, to humans by the bite of an anopheline mosquito.

Caption: An epiparasite is one that feeds on another parasite. This relationship is also sometimes referred to as hyperparasitism which may be exemplified by a protozoan (the hyperparasite) living in the digestive tract of a flea living on a dog.
Movement of Virus into Hosts: Infection
Virus enters the body at several sites called portals of entry.
The four major portals of entry:
1. Skin
2. Mucous membranes
3. Placenta
4. Parental route
To gain entry to the body, viruses must either
1. Infect cells in one of these surfaces,
2. Otherwise breach the surface (by trauma, the bite of an arthropod or animal, or injection, transfusion or transplantation), or
3. Be transmitted congenitally.
Viruses escape from the body via the same surfaces, often but not necessarily by the route used as a portal of entry.
The four major portals of entry:
1. Skin
2. Mucous membranes
3. Placenta
4. Parental route
To gain entry to the body, viruses must either
1. Infect cells in one of these surfaces,
2. Otherwise breach the surface (by trauma, the bite of an arthropod or animal, or injection, transfusion or transplantation), or
3. Be transmitted congenitally.
Viruses escape from the body via the same surfaces, often but not necessarily by the route used as a portal of entry.
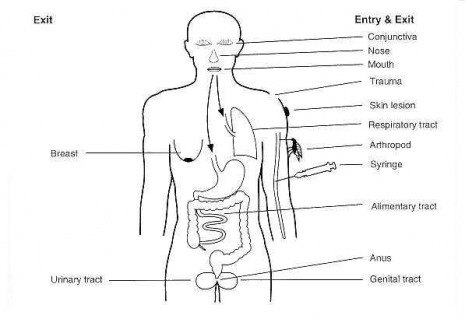
Caption: The portals of entry and exit for viruses into a human.
Portals of Entry
SKIN
Intact skin has a tough outer layer of cornified cells. This barrier protects the body from infection, but is frequently breached by trauma or by inoculation (e.g., by a needle or an insect bite). Some pathogens can enter via hair follicles, sweat glands, cuts, or bruises.
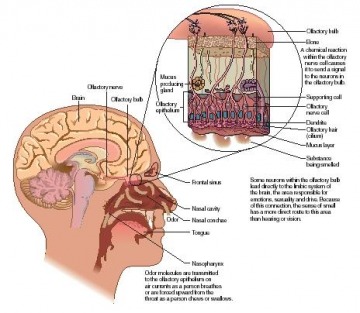
MUCOUS MEMBRANES
The mucous membranes are linings of mostly endodermal origin, covered in epithelium, which are involved in absorption and secretion.
Mucous membranes line all the body cavities:
- Respiratory
- Gastrointestinal
- Urinary
- Reproductive
- Conjunctiva (eyes)
Unlike skin, mucous membranes are thin, moist, and warm, and cells are living. They have the perfect environment for the growth of bacteria and viruses.
Mucous membranes line all the body cavities:
- Respiratory
- Gastrointestinal
- Urinary
- Reproductive
- Conjunctiva (eyes)
Unlike skin, mucous membranes are thin, moist, and warm, and cells are living. They have the perfect environment for the growth of bacteria and viruses.
PLACENTA
Pathogens can cross placenta and infect the foetus, resulting in
- Spontaneous abortion
- Birth defect
- Premature birth
- Spontaneous abortion
- Birth defect
- Premature birth
PARENTERAL ROUTE
Pathogens are deposited via punctures (nail, thorn, hypodermic needle), bites, cuts, stab wounds, or surgery.

Portals of Exit
Pathogens leave infected people to infect others. They often escape from the body via the same surfaces, but not necessarily by the route used as a portal of entry.
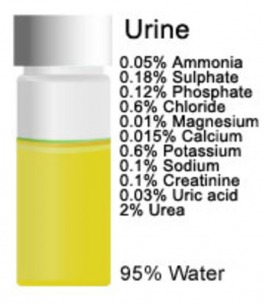
Pathogen leave host via:
- Secretion (tears, saliva, vaginal, semen, etc.)
- Excretion (faeces, urine)
Pathogen leave host via:
- Secretion (tears, saliva, vaginal, semen, etc.)
- Excretion (faeces, urine)